Day :
- Pediatric-Neonatal Gastroenterology and Nutrition
Location: Meeting Room no. 2
Chair
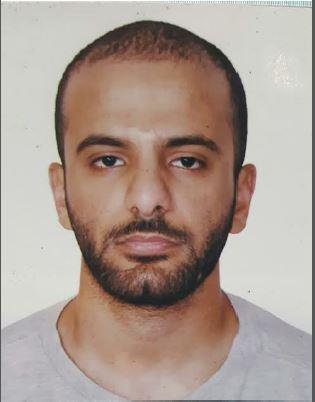
Ahmad Almaiman
King Khalid University Hospital, KSA
Session Introduction
Ahmad Almaiman
King Khalid University Hospital, KSA
Title: Pediatric pancreatitis: An overview with minor differences

Biography:
Dr. Ahmad Almaiman is an MBBS graduate from the University of Sharjah College of Medicine in the UAE. He conducted his internship in King Khalid University Hospital in Riyadh, Saudi Arabia, after which he became a licensed General Practitioner under the Saudi Commission for Health Specialties as well as a listing in the Dubai Medical Registry in the UAE. His field of interest is Pediatrics and sub specialties of interest and previous publishing include Neonatology and Gastroenterology.
Abstract:
Pancreatitis is defined as the inflammation of the pancreas. Alongside providing the regulatory hormones of insulin and glucagon, this organ aids in the digestion process by producing activated enzymes that exist near the duodenum. However, during an inflammation the enzymes self-digest the pancreas as a result of the acinar cell damage due to particular triggers. The incidence of acute pancreatitis has been increasing over the past twenty years; though the approach of managing it is similar to that of adult pancreatitis there still remains a need to convey official guidelines for pediatric management. It is convenient to understand the minor distinctions that relate to the cause and overall observation of pancreatitis as well as also being aware of any onward possible complications. Both gallstones and alcohol represent the two most common causes of pancreatitis in adult groups; while the former alongside hereditary pancreatitis and trauma are the lead causes of childhood pancreatitis. Viruses were at a previous time the mainstay in cases of acute pancreatitis but now they are intermediate. In spite of providing the same treatment used on adults there still exists a significant association with morbidity. Currently pediatric guidelines are being discussed, while adult guidelines remain in adequate service in the modern clinical setting of acute pancreatitis.
- Pediatric-Neonatal Gastroenterology and Nutrition
Session Introduction
Ahmad Almaiman
King Khalid University Hospital, KSA
Title: Pediatric pancreatitis: An overview with minor differences

Biography:
Dr. Ahmad Almaiman is an MBBS graduate from the University of Sharjah College of Medicine in the UAE. He conducted his internship in King Khalid University Hospital in Riyadh, Saudi Arabia, after which he became a licensed General Practitioner under the Saudi Commission for Health Specialties as well as a listing in the Dubai Medical Registry in the UAE. His field of interest is Pediatrics and sub specialties of interest and previous publishing include Neonatology and Gastroenterology.
Abstract:
Pancreatitis is defined as the inflammation of the pancreas. Alongside providing the regulatory hormones of insulin and glucagon, this organ aids in the digestion process by producing activated enzymes that exist near the duodenum. However, during an inflammation the enzymes self-digest the pancreas as a result of the acinar cell damage due to particular triggers. The incidence of acute pancreatitis has been increasing over the past twenty years; though the approach of managing it is similar to that of adult pancreatitis there still remains a need to convey official guidelines for pediatric management. It is convenient to understand the minor distinctions that relate to the cause and overall observation of pancreatitis as well as also being aware of any onward possible complications. Both gallstones and alcohol represent the two most common causes of pancreatitis in adult groups; while the former alongside hereditary pancreatitis and trauma are the lead causes of childhood pancreatitis. Viruses were at a previous time the mainstay in cases of acute pancreatitis but now they are intermediate. In spite of providing the same treatment used on adults there still exists a significant association with morbidity. Currently pediatric guidelines are being discussed, while adult guidelines remain in adequate service in the modern clinical setting of acute pancreatitis.
Ahmad Almaiman
King Khalid University Hospital, Riyadh, KSA
Title: Intussusception: Highlighted Aspects

Biography:
Dr. Ahmad Almaiman is an MBBS graduate from the University of Sharjah College of Medicine in the UAE. He conducted his internship in King Khalid University Hospital in Riyadh, Saudi Arabia, after which he became a licensed General Practitioner under the Saudi Commission for Health Specialties as well as a listing in the Dubai Medical Registry in the UAE. His field of interest is Pediatrics and sub specialties of interest and previous publishing include Neonatology and Gastroenterology.
Abstract:
Intussusception is a clinical disorder characterized by the telescoping of a proximal part of the bowel into its distal part. The point that invaginates into its adjacent part is known as the "Intussusceptum" (also referred to as the lead point), while the distal segment that receives the folding is known as the ''Intussuscipien''. This is one of the most important causes of acute abdomen in children, particularly infants and toddlers (3 months - 3 years), however it is a rare condition in adults and brings about a variety of symptoms and patterns; be it acute, intermittent, or chronic. This disorder particularly triggers worrisome matters that are deemed target worthy in the clinical setting. One of these matters is managing the possible shock that comes about with the excessive compromise of the mesenteric blood supply, which ends up thickening the intestinal wall leading to fatal complications of ischemia and perforation. Intussusception's diagnostic approach also happens to be its therapeutic approach, which is non-operative reduction (be it air or barium enema). The recurrence risk of Intussusception is one that demands a cautious observation in an in-patient setting, as the reduction management helps in limiting said risk allowing the recurrence to alter between 24 and 48 hours onwards. In recent years, there has been a presentation of this disorder in children who were provided with the Rotavirus vaccine bringing about different post-marketing surveillances to understand the possible risks of developing Intussesception. Along with the general overview on the topic of Intussusception the following highlights will be included: an emphasis on the potential complications of Intussesception, its distinguishing presentation between children and adults, favoring air over liquid enema in reduction management, and Intussesception's increasing risk if/when the Rotavirus vaccine is given.
- Gastrointestinal Disorders and Symptoms
Session Introduction
Romualdas Maskelis
National Cancer Institute, Lithuania
Title: Management of endoscopic treatment of gastrointestinal perforations, leaks and fistulae

Biography:
Romualdas Maskelis is currently working in National Cancer Institute, Lithuania.
Abstract:
Surgical treatment has been the mainstay for the management of GI leakage from perforations, fistulae, or anastomotic dehiscence. Moreover, in the era of minimal invasive surgery, the need for endoscopic management is increasing. The use of new endoscopic closure devices such as the endoscopic suturing system and over-the-scope clip allows endoscopicts to expand the indications of endoscopic treatment. Gastrointestinal (GI) leakage, fistulae and perforations can be seriously and life threatening. There has been a paradigm shift in the management approach of these conditions, from surgical to conservative, including endoscopic management. The systematic review of the literature form 1966 to 2013 for studies that have been published on endoscopic closure of perforations is found more than 700 studies but only included 24 cohort studies (21 retrospective , 3 prospective) in the analysis. In the past years, covered self-expanding metal stents were the mainstay of endoscopic therapy. However, two new techniques are now available that enlarge the possibilities of defect closure. In the past decades, endoscopic clip application has repeatedly been used as a minimally invasive treatment option for small leakages and fistulas of the upper GI tract. We applicate OTSC clips (OVESCO) more than for 30 patients during the last six year. Till now we don’t have randomized trials on OTSC application, and most authors provide retrospective case series with heterogeneous indications and applications. Most studies included less than 20 patients with gastrointestinal perforations. The OTSC obviously is a very effective treatment option of GI tract perforations, and in our opinion it is clearly superior to the placement of covered stents. Furthermore, in case of failure, the OTSC procedure does not impair further treatment, such as surgery. Further studies are needed to compare the novel techniques to other treatment modalities, and to define their exact place in treatment algorithms of upper GI perforations. Successful endoscopic closure of acute iatrogenic perforations in the GI tract can reduce medical costs and hospital stays and prevent the need for surgical intervention for the patient.
- Liver and Biliary Diseases
Session Introduction
Mohammed Shafiqul Islam Bhuiyan
US-Bangla Medical College and Hospital, Bangladesh
Title: Isolated hepatosplenic tuberculosis: A rare case report
Time : 16:00-16:40

Biography:
Mohammed Shafiqul Islam Bhuiyan has completed his MD in Gastroenterology from Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh. He is currently working as an Associate Professor and Head of the Department of Gastroenterology, US-Bangla Medical College, Narayanganj, Bangladesh.
Abstract:
Tuberculosis is common in Bangladesh. It rarely involves the liver and spleen and when it does so, it is usually associated with disseminated disease. This is case report of a patient with isolated tuberculosis of the liver and spleen. A 55 years old female presented with fever with chill and rigor and upper abdominal pain. USG revealed multiple hypoechoic lesions with central echogenicity in liver and spleen. CT scan showed multiple mixed density lesions in the liver and spleen. AFP, CEA and CA-19-9 were normal. As temperature was not subsided with antibiotics, pus from liver and spleen was aspirated and sent for gram and AFB stain, C/S, malignant cell and Gene Xpert. All but Gene Xpert reports were negative. A detailed workup failed to identify other focus of tuberculosis. CAT-1 Anti tubercular started and the fever subsided. The patient gained weight on the subsequent follow up. Tuberculosis should also be considered in the differential diagnosis for multiple nodules in the liver and spleen along with other diagnosis, though it is rare. Gene Xpert is a good diagnostic tool.
A.K.M Shafiqul Islam
BIRDEM General Hospital, Bangladesh
Title: Correlation between serum complement C3 and FIB4 Index with stages of fibrosis of liver by fibroscan in NAFLD patients

Biography:
Abstract:
Introduction & Objective: Despite the high prevalence of NAFLD non-invasive markers of disease activity and severity remain limited. Different modalities are available for predicting severity of NAFLD with different sensitivity and specificity. A single, cheap, widely available marker with high sensitivity and specificity is yet to be identified. The current study intends to find out the utility of serum complement C3 and FIB4 Index to predict stages of fibrosis of liver in NAFLD patients.
Method: This observational cross-sectional study was done at department of GHPD, BIRDEM General Hospital, Dhaka, during the period of January 2016 to October 2017. A total of 105 sonographically diagnosed NAFLD subjects attending at OPD and admitted in that Hospital were included in the study. Statistical analysis was done with SPSS version 16.
Result: Out of 105 subjects, 70 (66.7%) were female and 35 (33.3%) male. Serum complement C3 (mg/dl) 142.30±21.02 (mean±SD). USG of W/A or HBS showed 61 (58.10%) had grade I, 33 (31.43%) grade II, 11 (10.48%) grade III fatty liver disease. Fibroscan showed no fibrosis in 31 (29.52%), F1 stage of fibrosis in 22 (20.95%) and F2 in 22 (20.95%). FIB4 Index was 1.22±0.76 (mean±SD). Pearson correlation test showed stages of fibrosis by fibroscan had significant positive correlation with FIB4 index, weak positive correlation with BMI (kg/m2), weak negative correlation with serum complement C3 and almost no correlation with grading of fatty liver on USG (Spearman’s correlation).
Conclusion: The positive correlation of stages of fibrosis by fibroscan with FIB4 index was significant whereas negative correlation with serum complement C3 was not so significant statistically. Sensitivity and specificity of serum complement C3 and FIB 4 index as fibrosis marker was not so significant. Serum complement C3 and FIB4 index may not be used as a marker of severity of fibrosis.
- Gastrointestinal Carcinogenesis and Therapeutics
Location: Meeting Room no. 2
Session Introduction
Romualdas Maskelis
National Cancer Institute, Lithuania
Title: Risk of second primary malignancy after early cancer endoscopic resection

Biography:
Romualdas Maskelis is currently working in National Cancer Institute.
Abstract:
Today, there is a growing tendency for second or even Primary Early Gastric Cancer (PEGC) after Endoscopic Submucosal Disorder (ESD) or Mucosal Resection (EMR). The PEGC is earlier, until there is no visible or unnoticed violation in the clinical period, but as it really was, there is no possibility or at least it would be difficult to retrospectively evaluate it. It is clear that today's endoscopic diagnostic of PEGC has improved significantly, and today we can already see cancer when it is in the mucous membrane or in the submucosal layer, only long term and indefinitely endoscopic observation is required. Several retrospective studies have shown excellent long-term results in patients with PEGC, who had endoscopic intervention on stomach cancer. It is reported in the literature that the incidence of PEGC after ESD/EMR is higher than in patients undergoing gastrectomy. Longer life expectancy and PEGC-it is the risk factors independent of one another. Most of the lesions were found at an early half-yearly or annual follow-up and were successfully treated endoscopically, with excellent long-term results. The H. pylori eradication particularly reduces the risk of PEGC. Prolonged life expectancy and polymorphic (metachromic) PEGC are independent of each other, and most of the lesions were found at an early half-yearly or annual follow-up and were successfully treated endoscopically with excellent long-term results, and eradication of H. pylori particularly reduces the risk of PASV. Today, we have an agreement based on previous observations-if stomach cancer becomes occurred within one year after ESD is considered to be missed syndrome of stomach cancer. Four patients with PEGC who were treated endoscopically in Lithuanian NCI since 2016- for two was perform ESD and two were undergo to surgery. Unequivocally, endoscopic operations are now well advanced and doctors performing ESD/EMR are certified (expert status) and institutions are ranked by the number of such interventions per year. In the West, where both morbidity and mortality are higher than in Japan, where early mucosal cancer with high dysplasia is recognized as a cancer. Now any from us thinking about implementing a gastric cancer screening program, as was made in S. Korea where more 40 % patients were treated endoscopically. Today, we already have a risk assessment strategy for PASVs, but are needed for endoscopic monitoring regimes and in the near future the national gastric cancer screening program.
